Why you should be worried about infectious diseases like novel coronavirus pneumonia
The case fatality rate (CFR) of novel coronavirus pneumonia (NCP) was reported to be 2.6%, much lower than SARS, which had a CFR of 9.6%. Because of its relative low CFR, many people including the Chinese authorities were ignorant of its danger. In this post, I will show you that an infectious disease can be a disaster simply because of its high transmission rate regardless of its power of killing people. Indeed, this kind of highly transmissible diseases can lead to humanitarian crises, which can destroy a whole nation, race, or civilization.
To understand this, it is as simple as to check the following two statements:
- Without intervention, a highly infectious disease can infect a majority of the population.
- The therefore exhausted medical care system leaves the infected untreated, and then the fatality rate skyrockets.
An infectious disease can infect a majority of the population
This terrifying statement is surprising and, somewhat, counter-intuitive. We have known of many infectious diseases, but you have never suspected whether the people around you are infected. If an infectious disease can infect more than 50% of the population, this will imply that more than one half of the people around you are infected. It is like that I am telling you that one half of your classmates or colleagues are aliens.
Well, they may not be aliens, but some mathematical model predicts that they may be infected. The Susceptible-Infectious-Removed (SIR) model provides us an insight on how a small group of infected people eventually infect the majority of the population. The SIR model is a very basic one, and it only considers short-term outbreaks, where the natural birth and death can be ignored. Despite its simplicity, it is powerful enough for us to understand the danger of a highly infectious disease.
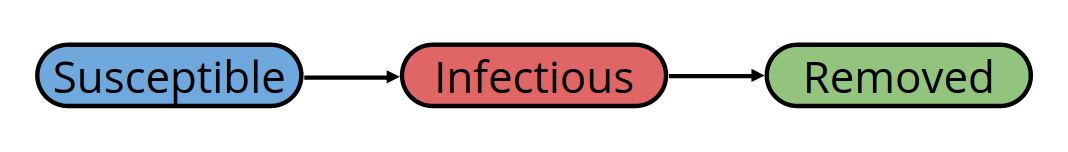
The SIR model divides the population into three compartments: susceptible, infectious, and removed.
- A susceptible is someone who can be infected but not yet infected.
- An infectious is someone who has been infected and can infect the susceptible.
- A removed is an infectious who has either recovered (and obtained immunity) or died; in either case, he can no longer infect others.
With time evolving, the susceptible gradually get infected and then gradually get removed. I will omit the math here and instead use the following figure to illustrate the disease outbreak.
In each of the above (equivalent) figures, we can observe two stages.
- In the first stage, when the majority are susceptible, the number of infectious rises dramatically (red line).
- Then, it reaches its peak, where many people have either recovered or died and the disease no longer has that many susceptible to infect, the number of infectious drops (red line).
Although the disease dies out eventually, about 80% percent of the population have been infected during the course.
Now, let me tell you that this disease is not even that highly transmissible: At the beginning of the outbreak, each infectious infects only two susceptible in average. That is, the basic reproduction rate of this disease is 2. It is evident that a higher basic reproduction rate will result in a higher total number of infected.
With this information, you can already infer the danger of a highly transmissible disease. In the above case, for a population of 1 billion, a fatality rate of as low as 1% implies 8,000,000 deaths!
Too little medical resources for too many infected
Previously, I assumed a low fatality rate of 1%. This assumption was based on another assumption that there were sufficient medical resources for every infected. What if this is not the case?
The following figure shows the evolution of the number of infectious for various basic reproduction rate $R_0$. For instance, a basic reproduction rate of 4 means that every infectious infects 4 susceptible in average at the beginning of the epidemic (this number will decrease with the drop of the density of the susceptible).
From this figure, we can observe that the higher the basic reproduction rate is, the higher and the earlier the epidemic peak will be. In particular, for a disease with a basic reproduction rate of 4, at the peak, 40% of the whole population are infectious and thus need medical care.
This raises the question: is there any city in the world able to provide medical care of this scale?
According to OECD, there are 3.4 doctors per 1,000 population in the world. Qatar has the highest relative number of doctors, with its 7.7 physicians per 1,000 people. Let us optimistically assume that in a rich village with a population of 1,000 there are 10 doctors (triple the number of the OECD average). Then, during the epidemic peak, each doctor should treat 40 patients per day, which amounts to 5 patients per hour, or 1 patient per 12 minutes (assuming that he works 8 hours per day).
The number of medical workers is not the only concern. To accommodate all these 400 patients, the hospitals will need a total of 400 beds. That is, 40% percent of the population sleep in the hospital. At this rate, the hospital might as well be called a hotel. In fact, during such an epidemic, most patients will stay at home (or in the church), and the doctors visit them day by day and give them only basic medical care. Not only the doctors, but also the relatives and many volunteers will be involved in this fight against the epidemic. If you are interested, I strongly recommend Albert Camus’s novel La Peste (The Plague in English).
The take-home message here is that no government is able to handle this kind of epidemic because the medical care system is not designed for this purpose in the first place. In fact, this kind of unrealistic medical care system would only be a waste in the absence of epidemic.
The consequence is that many patients cannot obtain adequate medical care and die, and that the fatality rate becomes much higher than when there are enough medical resources for every patient. This phenomenon was common during the Middles Ages but would be called humanitarian crisis in the modern time. It is understandable that the population will be panic.
That is essentially why the whole world needs to pay close attention to novel coronavirus and to help the Chinese people. The Chinese people are in great crisis! They need your help!
What lesson can we learn from novel coronavirus pneumonia?
Since it is inefficient to fight the infectious disease when there is already an outbreak, it becomes critical to prevent its outbreak since the beginning. Early detection and quick response are the key here.
In the figure below, the red solid line represents the number of infectious for a disease with a basic reproduction rate $R_0=4$ in the current world. The red dotted line represents an alternative world where $R_0=2$. In the alternative world, the epidemic peak is much lower than in the current world; also, the duration to reach the peak is much longer than in the current world.
In the current world, if we can detect the ongoing epidemic, we can then take measures to reduce $R_0$ to 2 and therefore change our future. We hence change the course of the world line and move toward some altered world (marked as the purple and the violet dashed line for early detection and late detection respectively). In the altered worlds, the peak is only as high as in the alternative world, and it also happens later than the current world, good news for the suffering population.
Moreover, the slope in the altered worlds is much less steep than the current world, which implies that its shock to the medical care system and the economy is less significant. This gives the government more time and room to prepare themselves (e.g. produce medical resources) as well as to motivate people to fight against the epidemic together. The earlier the detection is, the less difficulty will await us.
How to reduce the basic reproduction rate $R_0$?
Now the only remaining question is whether we can reduce $R_0$? To answer this question, it would be helpful to understand the fact that $R_0$ depends not only on the characteristic of the disease itself but also on the habit and behavior of the population. Basically, there are two major approaches to reduce $R_0$: reducing the transmission probability and early quarantine.
Reducing the transmission probability ($\beta$)
The key to reduce the transmission probability is to identify the transmission itself. For a disease transmitted via droplets (e.g. SARS), the face mask and the habit of washing hands become essential. For a disease transmitted via intercourse (e.g. AIDS), the condom and the habit of fixed partnership become essential. For a disease transmitted via a vector (e.g. malaria), the killing of the vector in question becomes essential.
Early quarantine ($\gamma$)
If we can quarantine an infectious before he could ever infect any susceptible, then we successfully reduce $R_0$, by definition. If we can quarantine all infectious at a given moment $t$, we can stop the epidemic immediately at this exact moment.
In practice, we are not God and thus are not able to achieve this. It is not obvious whether a certain person is infectious; the word “infectious” is not written on his face. Even if this word was written on his face, before you could locate him he might have already infected several people.
Although we cannot achieve 100% quarantine, a partial quarantine is still of much help. For a disease with $R_0 = 4$, if we manage to quarantine 50% of the infectious before they could ever infect any others, we then successfully reduce $R_0$ to 2. This is also why I emphasized, in the previous section, the early detection of the epidemic: the earlier the detection is, the easier the quarantine will be (see the following figure).
Summary
An infectious disease can be dangerous either because of its high fatality rate alone or because of its high transmission rate alone. The former makes a death verdict to the infected; the later exhausts the public medical resources and leaves the infected untreated. The former hits on individuals and families; the latter hits on the whole society.
To prevent the outbreak of the disease, early detection is the key. Following the detection, measures should be taken to reduce the basic reproduction rate. The two major approaches to reduce the basic reproduction rate are reducing the transmission probability and early quarantine.